Multimodal approaches have been demonstrated to allow enhanced pain control without the dependence on opioids. Pain control can be validated through measures after surgery procedures regarding tissue damage. Joint Commission on Accreditation of Healthcare Organizations (JCAHO) evaluated pain in 4 measures: 1) intensity, 2) quality, 3) effect on function and quality of life, 4) objective assessment of amount of pain medication being used. A search was conducted for recent literature on PubMed.gov using the search terms opioids, pain management, and best practice. This is a review on an article based on multimodal approaches to evaluate postoperative pain.
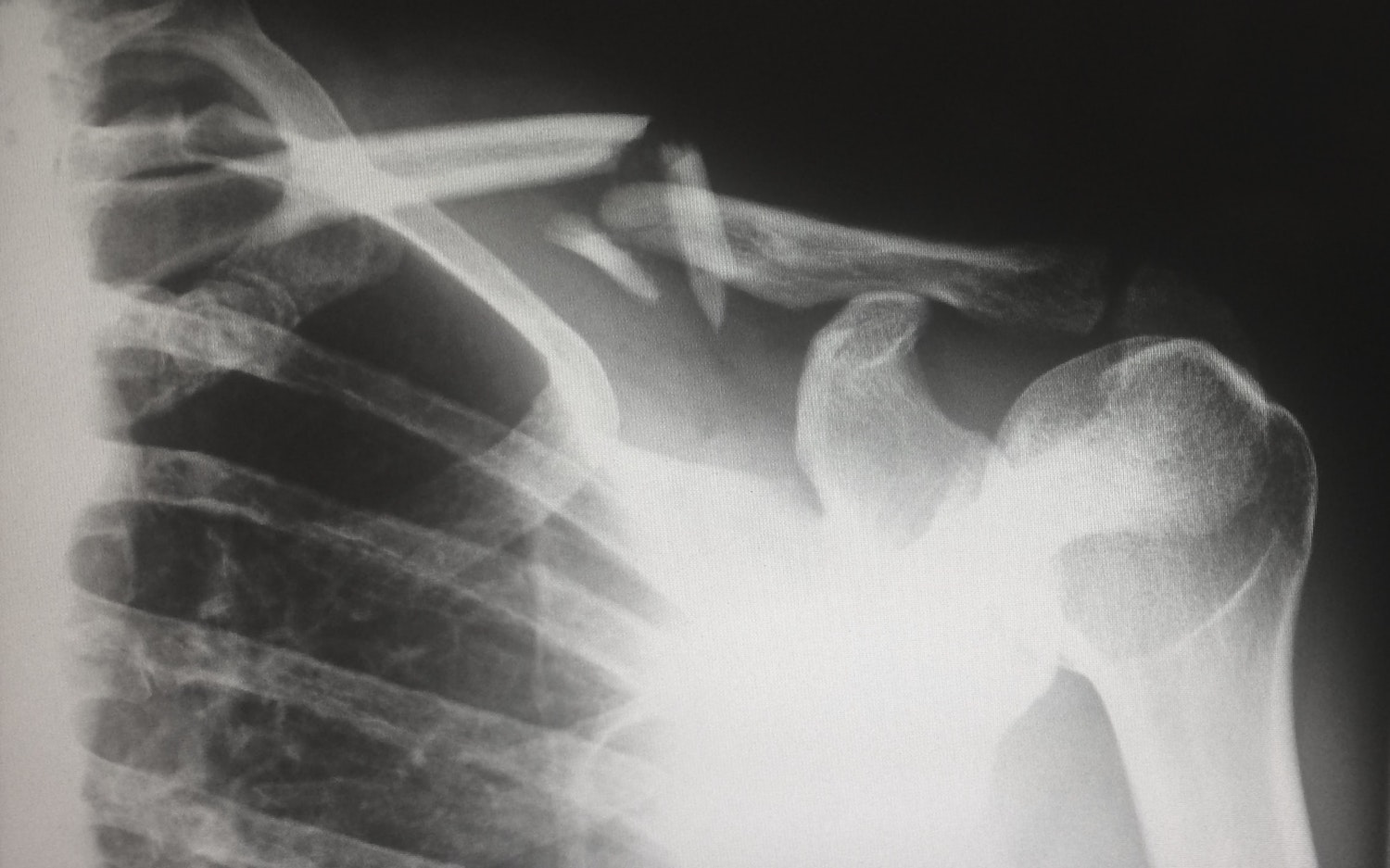
An abuse of opioid medication in pain management after postoperative pain can lead to adverse side effects as confusion, urinary retention, ileus, respiratory depression and death. Multimodal pain management has been pushed for in replacement for decrease opioid consumption. Pain management controlled in a poor manner leads to reduced patient mobility, increase deep vein thrombosis, pulmonary embolus, and pneumonia, respectively. Multimodal pain management reduces both postoperative pain and opioid consumption. Figure 1 below demonstrates different amounts of opioid use. Table 1 represents an approach and evidence data using the multimodal approach for pain management.
Figure 1. Opioid Consumption
Table 1. Approach and evidence data using the multimodal approach for pain management.
| Agent | Source | Design type | Key findings |
| Preemptive analgesia | Lee et al. [21] | Prospective observational clinical study | Significant improvement in immediate postoperative pain as well as usual activity, depression/anxiety and self-care at 2 weeks postoperatively in patients undergoing preemptive analgesia protocols. |
| NSAID | Roberts et al. [31] | Cochrane review | Cyclooxygenase-2 inhibitors are effective in providing analgesia in the extended postoperative period following orthopedic surgery with a minimal side effect profile. Nonselective NSAID provide effective analgesia, with greater benefits observed with longer treatment duration. |
| Gabapentinoids | Khurana et al. [33] | Randomized controlled trial | Pregabalin was associated with less pain intensity and improved functional outcomes 3 months after lumbar discectomy followed by gabapentin and then placebo. Pregabalin and gabapentin reduced the amount of opioid consumption versus placebo. |
| Gabapentinoids | Yu et al. [34] | Systematic review and meta-analysis | In pooled analysis, both gabapentin and pregabalin significantly reduced the postoperative narcotic consumption |
| Acetaminophen | Cakan et al. [36] | Randomized controlled trial | Scheduled intravenous acetaminophen was associated with improved pain scores and greater patient satisfaction with pain control than placebo. There was no difference in narcotic usage between treatment and control cohorts. |
| Acetaminophen | Khalil et al. [38] | Randomized controlled trial | Both preventive and preemptive acetaminophen enhanced analgesia and decreased postoperative analgesic consumption |
| Muscle relaxants | Van Tulder et al. [40] | Cochrane review of randomized controlled trials | Strong evidence that muscle relaxants are more effective than placebo for patients with acute low back pain on short-term pain relief. No studies to date have directly assessed the effect of muscle relaxants in postoperative spine patients. |
| Ketamine | Loftus et al. [44] | Randomized controlled trial | Intraoperative ketamine reduced opiate consumption in the 48 h postoperative period in opiate-dependent patients with chronic pain. This benefit was observed with no increase in side effects. |
| Ketamine | Subramaniam et al. [45] | Randomized controlled trial | No difference in pain scores at rest and movement was noted between the treatment and placebo groups. Patients in treatment and placebo groups required similar amounts of narcotics in 48 h postoperative period. |
| Neuraxial blockade (epidural) | Guilfoyle et al. [49] | Randomized controlled trial | Lower early postoperative VAS pain scores within the treated group. More patients in the fentanyl group required temporary urinary catheterization. |
| Neuraxial blockade (intrathecal) | Ziegeler et al. [50] | Randomized controlled trial | Patient-controlled analgesia requirements were significantly lower in the treatment group. |
| Neuraxial blockade (intrathecal) | Chan et al. [51] | Randomized controlled trial | Patients who received fentanyl demonstrated a significant decrease in their mean pain VAS, an increase in the time to first PCA bolus and a 41% reduction in the total PCA morphine received. No patients had respiratory compromise requiring treatment. |
| Extended-release local infiltrative anesthetics | Bramlett et al. [58] | Randomized controlled trial | Treatment with DepoFoam bupivacaine 532 mg was associated with statistically significantly greater analgesia while patients were at rest after surgery compared with bupivacaine HCl. |
HCl = hydrogen chloride, NSAID = nonsteroidal anti-inflammatory drugs, PCA = patient-controlled analgesia, VAS = visual analogue scale.
Table 2. Multimodal treatment agents of postoperative pain according to North American Spine Society with evidence grades.
| Agent | Evidence Grade |
| Preemptive analgesia | Grade B fair evidence |
| NSAID | Grade B fair evidence |
| Gabapentinoids | Grade A good evidence |
| Acetaminophen | Grade A good evidence |
| Muscle relaxants | Grade I insufficient evidence |
| Ketamine | Grade I insufficient evidence |
| Neuraxial blockade (intrathecal, epidural) | Grade A good evidence |
| Extended-release local infiltrative anesthetics | Grade A good evidence |
NSAID = nonsteroidal anti-inflammatory drugs.
Multimodal pain management has demonstrated improvements of pain control decreasing the consumption of opioid medications. Based on the literature provided, it provides evidence on common agents used for multimodal pain management treatment. Further research can look at increase patient populations and cohort assessment regarding opioid consumption and multimodal pain management.
Austin Spine & Wellness Center Text or Call (512) 501-1770
References
Devin, C. J., & McGirt, M. J. (2015). Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes. Journal of Clinical Neuroscience, 22(6), 930-938.